×
For Early Food Introduction
These sections contain the same information as in the PDF handouts throughout this section but are formatted for easier placement within EMR systems to place in after visit patient handouts.
Helpful Tips and Tricks for Allergy Prevention
Helpful Tips and Tricks for Allergy Prevention
The dual exposure hypothesis is a belief that the ability to eat a food without a reaction (tolerance) is developed by having the GI tract see the food, whereas the potential for food allergy is developed by skin exposure to the food, which can be worsened by eczema or skin breakdown. It is important to try to prevent repeated skin exposure to foods that your child has not eaten yet. To try to limit skin exposure it is best to avoid eating allergenic foods in your child’s play area and restrict eating to the table. It is important to clean surfaces where food is prepared or eaten to help reduce your child’s environmental exposure to any food allergens. Limit snacking throughout the house to reduce the amount of food dust/particles that get on rugs, carpets, etc. It is best to wash your hands before applying lotions and creams and after handling foods.
Peanut Introduction as per NIAID/LEAP
Why should I introduce peanut products to my baby so early in life?
Introducing peanut products to your baby early in life can help prevent him from developing a peanut allergy later on. Ask your doctor when it is right to introduce peanut products for the first time.
What should I do before giving my baby peanut products for the first time?
Talk with your baby’s doctor about whether he is ready to try peanut products.
If your baby has other known food allergies or very bad eczema (dry, scaly patches of skin), ask your doctor if your baby should have an allergy test or see a pediatric allergist (allergy doctor).
How do I introduce peanut products?
Safety tips
Give the first taste when your baby is healthy. Do not give the first taste if he has a cold, fever, diarrhea or other illness.
Give your baby his first taste of peanut products at home. Do not give the first taste at daycare or in a restaurant.
Timing tips
Set aside at least 2 hours after the first taste to watch your baby for a reaction. Make sure you or another family member can give full attention to your baby.
For the very first taste, give a small amount, the tip of a small spoon. Wait 10 minutes between the first and second taste. If your baby does not have any reaction after 10 minutes, give the rest of the peanut butter at his normal eating speed.
Give your baby 2 teaspoons (6 grams) of peanut products at least 3 times per week. This will help prevent him from developing a peanut allergy later in life.
Tips while your child eats:
Prepare a full serving of peanut butter from the recipe below.
Offer the first taste on a small spoon.
For babies and children under age 4, mix peanut butter with 1 safe food at a time. Do not give plain peanut butter to any baby or child under age 4.
Do not push your baby to eat more than he wants.
Peanut recipes for babies
Option 1: Peanut butter puree
You will need:
2 tsp. smooth, all-natural peanut butter (with no added ingredients)
2-3 tbsp. of plain yogurt or pureed (smooth) fruit or vegetable that your baby likes
Mix peanut butter and yogurt or fruit or vegetable puree. Add more water if you want the puree to be thinner.
Option 2: Peanut butter powder sauce
You will need:
2 tsp. powdered peanut butter or peanut flour
2-3 tbsp. of warm water, oatmeal, applesauce or mashed banana
Mix peanut butter or peanut flour with the water, oatmeal, applesauce or banana.
Let the mixture cool.
Add more water if you want the mixture to be thinner.
Option 3: Bamba® peanut butter puffs
You will need:
21 Bamba® peanut butter puffs
For babies aged 7 months and under, soften puffs in 4-6 tbsp. of water. Feed your baby one puff at a time.
For babies older than 7 months or who can eat dissolvable solids, feed puffs one at a time as normal.
A note about choking
Only give your baby smooth peanut butter.
Never give your baby chunky or crunchy peanut butter. Your baby can choke on the small peanut pieces.
Never give your baby whole peanuts or pieces of peanuts.
A note about food allergies
When your baby is trying a peanut product for the first time, it is important to watch him for signs of a food allergy. An allergic reaction can happen up to two (2) hours after trying a new food.
What is a food allergy?
A food allergy is when your body mistakes a certain food for something dangerous or unknown.
What are common signs of a food allergy?
Rash or hives (swollen red bumps) around the mouth or on the face or body
Swollen lips, tongue or face
Itching
Vomiting
Coughing
Change in skin color (blue or pale)
Wheezing (whistling sound when you breathe in)
Trouble breathing
Suddenly feeling tired or drowsy
Feeling like your body is going limp
What to do if your baby has an allergic reaction
Call 911 or take your baby to the emergency room right away.
If your baby’s allergist (allergy doctor) has created a Food Allergy Action Plan, follow the steps.
Helpful Tips and Tricks for Allergy Prevention
The dual exposure hypothesis is a belief that the ability to eat a food without a reaction (tolerance) is developed by having the GI tract see the food, whereas the potential for food allergy is developed by skin exposure to the food, which can be worsened by eczema or skin breakdown. It is important to try to prevent repeated skin exposure to foods that your child has not eaten yet. To try to limit skin exposure it is best to avoid eating allergenic foods in your child’s play area and restrict eating to the table. It is important to clean surfaces where food is prepared or eaten to help reduce your child’s environmental exposure to any food allergens. Limit snacking throughout the house to reduce the amount of food dust/particles that get on rugs, carpets, etc. It is best to wash your hands before applying lotions and creams and after handling foods.
Food Introduction (other than peanut)
It is best to introduce new foods to your child in an age-appropriate and culturally appropriate manner. The foods should be free of choking hazards, such as whole nuts and thinned by mixing them with formula, breast milk, or pureed fruits or vegetables. There is no reason to delay the introduction of foods that are considered “allergenic” like, tree nuts, eggs, dairy, soy, wheat, sesame, fish, and shellfish beyond 4-6 months of exclusive breat feeding. We recommend that you start with a tip of a teaspoon and double this every 10 to 20 minutes until your child has reached about 2 grams of the allergen protein. The amount of protein can be found on the nutrition label. For example, about 2 teaspoons for nut-butters, and sesame tahini) and about 1/3rd of a large egg have 2 grams of those specific proteins.
This initial food introduction can also be done more slowly if you or your provider have any concerns. It is important to be aware of the signs of an allergic reaction or anaphylaxis. These symptoms include hives, swelling, wheezing, cough, shortness of breath, nausea, vomiting, difficulty breathing, or loss of consciousness. If you have any concerns it is important to call 911. Please let your provider know if there are any signs of a reaction because a referral to an allergist will be made. If foods are tolerated it is important to keep them in the diet in regular intervals.
Videos for Parents for Peanut Introduction as per Addendum Guidelines
What Parents Should Know [English]: https://players.brightcove.net/6056665225001/5cmMqFpv5_default/index.html?videoId=6216466727001
What Parents Should Know [Spanish]:
https://players.brightcove.net/6056665225001/5cmMqFpv5_default/index.html?videoId=6216471682001
Introducing Complimentary Foods
When is an infant ready for solid food, and what foods are developmentally appropriate?
If serving purees, aim for a smooth, even texture for your baby’s first few foods. First finger foods given to an infant should be very soft and easy to smash between your thumb and forefinger. For thicker foods, such as nut butters, it is best to thin them out with warm water or mix them into something smoother, such as applesauce. Some signs that a baby is ready to try solid foods are:
- Good head and neck control
- Ability to sit on their own with minimal support
- Opens mouth and leans forward when offered food
- Able to grasp larger objects and bring them up to the mouth
Some infants may show developmental signs of readiness before age 6 months but introducing complementary foods before age 4 months – or waiting until after 6 months – is not recommended.
Nutrition Guidance for Children During their First 12 Months of Life
The American Academy of Pediatrics states that: “There is no evidence that delaying the introduction of allergenic foods, including peanuts, eggs, and fish, beyond 4 to 6 months prevents atopic disease.”
Why is infant nutrition so important?
During an infant’s first year of life, infants should receive adequate amounts of essential nutrients because these foods are needed for healthy brain development and overall growth. Also, establishing healthy dietary patterns early in life can influence eating behaviors and overall health throughout the course of life.
Key Recommendation
Between ages 0-4 months: Exclusive breastmilk and/or formula feeding
- What form of milk? Human breast milk, iron-fortified infant formula, or a combination of both
- Do I need to supplement the milk with anything?
- You may need to provide a vitamin D supplement, depending on which form of milk you choose
- For exclusive human breastmilk feeding, vitamin D supplement of 400 IU per day
- For breast milk/formula mixed feeding, vitamin D supplement of 400 IU per day
- For exclusive iron-fortified formula feeding, no vitamin D supplement is needed since infant formula is vitamin-fortified
Between 4-6 months: When your child is ready, start to introduce complementary foods
- How do I know when my child is ready?
- The ages infants show signs of readiness vary and are typically between ages 4 and 6 months.
- Signs that your child may be ready for complementary foods include:
- Being able to control the head and neck
- Sitting up alone or with support
- Bringing objects to the mouth
- Trying to grasp small objects, such as food or toys
- Swallowing food rather than pushing it back out onto the chin
- Swallowing food rather than pushing it back out onto the chin
- There is no evidence that delaying the introduction of allergenic foods helps prevent food allergy (Please see information specific to high-risk infants below)
Between 6-12 months: Introduce complementary foods no later than 6 months
- What complementary foods should I give my child?
- Infants should be encouraged to consume a variety of complementary foods
- Introduce iron-rich foods: meats seafoods, iron-fortified infant cereals
- Introduce zinc-rich foods: meats, beans, zinc-fortified infant cereals
- Introduce a variety of foods from all food groups: protein, fruits and vegetables, dairy, grains
- Introduce potentially allergenic food groups: egg, dairy, peanuts, tree nuts, soy, shellfish, fish, wheat, sesame.
How do I know if my child is at high risk of developing a peanut allergy?
- Risk factors: If your child has severe eczema, egg allergy, or both, s/he may be at a higher risk of developing a peanut allergy
Recommendations: age-appropriate, peanut-containing foods should be introduced to the diet as early as age 4 to 6 months.
Establishing Healthy Dietary Patterns in an Infant’s First Year of Life
Dietary Components to encourage:
- A wide variety of fruits, especially berries and whole fruits
- A wide variety of vegetables from each vegetable group, which includes dark green (ex. broccoli), red/orange (ex. carrots), legumes (i.e., beans, peas, lentils), starchy vegetables (ex. potatoes)
- Whole grains
- Unprocessed meat
Dietary Components to limit:
- Processed meats (ex. cold cuts)
- Refined grains
- 100% fruit juice
- Foods with high sodium content
- Foods containing added sugars
Dietary Components to Avoid:
- Honey and unpasteurized foods and beverages
- Sugar-sweetened beverages (ex. soda, sweet tea)
- Liquid cow’s milk, fortified soy beverages, and milk alternatives (such as plant-based milk) in place of breast milk or infant formula
- Caffeinated beverages
- Seafood with high mercury content
- Loose nuts and other choke-risk foods
Introducing your child to the 9 major allergens:
The 9 major potentially allergenic foods should be introduced as complementary foods. There is evidence that introducing peanut-containing foods in an infant’s first year of life can reduce the risk that s/he will develop a peanut allergy There is no evidence that delaying introduction of allergenic foods beyond 6 months prevents food allergy.
- Dairy
- Egg
- Peanuts
- Tree Nuts
- Soy
- Wheat
- Fish
- Shellfish
- Sesame
Dot phrases modified from PDF found at: https://famp-it.org/wp-content/uploads/aap-statement-FAMPIT_Nutrition-Education_less12mo.pdf
Nutrition Guidance for Children After Their First Birthday
Nutrition Education Adapted from the 2020-25 Dietary Guidelines’ New Chapter on Infant and Toddler Nutrition
Following healthy dietary patterns early on is important for maintaining proper growth, and nutritional needs, and reducing the risk for chronic disease later in life. You can help your child establish healthy eating habits by encouraging them to eat a variety of nutrient-dense foods from all the food groups. You can start by replacing less healthy snacks and ingredients with nutrient-dense alternatives!
Dietary Components to LIMIT:
- Processed meats (e.g., cold cuts)
- Foods with high sodium content
- Food containing added sugars
- 100% fruit juice, even if it doesn’t have added sugar
Dietary Components to AVOID:
- Sugar-sweetened beverages (e.g., soda, juice drinks, sports drinks)
- Caffeinated beverages
- Alcoholic beverages
- Seafood with high mercury content
- Loose nuts and other choke-risk foods
It is important to choose nutrient-dense foods from each food group!
- Fruit
- All fresh, frozen, canned in 100% fruit juice, and dried fruits
- Examples: apples, pears, oranges, grapefruit, berries (i.e., blueberries, raspberries, strawberries), bananas, melons, peaches, plums, raisins, papaya, pomegranate
- Encourage whole fruits, limit fruit juice to 4 ounces per day
- Veggies
- Dark Green Vegetables: broccoli, bok choy, collards, kale, mustard greens, spinach
- Red & Orange Vegetables: carrots, pumpkin, squash, bell peppers, sweet potatoes, tomatoes
- Beans, Peas, Lentils: black beans, garbanzo beans, edamame, kidney beans, lentils, split peas, pinto beans
- Starchy Vegetables: plantains, white potatoes, corn, yam, yucca, water chestnuts
- Other Vegetables: asparagus, beets, Brussels sprouts, cauliflower, green beans, eggplant, cucumber, turnips, seaweed
- Dairy
- All fluid, dry, or evaporated milk (includes lactose-free/reduced products and fortified soy beverages)
- Examples: milk, buttermilk, yogurt, kefir, cheese
- Limit cream, sour cream, frozen yogurt, ice cream, and cream cheese
- Grains
- Whole grains: brown rice, oats, quinoa, whole-grain cereals/crackers, dark rye, barley (not pearled), whole-grain cornmeal, whole-wheat bread
- Refined grains: white rice, white breads, refined-grain cereals/crackers, pasta, cream of wheat/rice, corn grits
- Encourage whole grains, limit refined grains
- Protein
- Meats, Poultry, Eggs: beef, goat, lamb, pork, chicken, duck, goose, turkey, organ meats, chicken eggs and other birds’ eggs
- Seafood: anchovy, black sea bass, clams, cod, crab, flounder, haddock, lobster, oyster, salmon, sardine, scallop, shrimp, sole, squid, light tuna
*avoid seafood high in mercury
- Nuts, Seeds, Soy: tree nuts, peanuts, nut butters, seeds, seed butters, tofu, tempeh, soy protein isolate, soy concentrate
Dot phrases modified from PDF found at: https://famp-it.org/wp-content/uploads/FAMPIT_Nutrition-Education_more12mo.pdf
Early Introduction of Complementary Foods
Which foods should my patient eat, and how much?
The American Academy of Pediatrics states that: “There is no evidence that delaying the introduction of allergenic foods, including peanuts, eggs, and fish, beyond 4 to 6 months prevents atopic disease.”
When counseling families on food introduction, it is important to discuss how to tell when an infant is ready for solid food and what foods are developmentally appropriate. If serving purees, families should aim for a smooth, even texture for the baby’s first few foods. First finger foods given to an infant should be very soft and easy to smash between the thumb and forefinger. For thicker foods, such as nut butters, it is best to thin them out with warm water or mix them into something smoother, such as applesauce. Some signs that a baby is ready to try solid foods are:
- Good head and neck control
- Ability to sit on their own with minimal support
- Opens mouth and leans forward when offered food
- Able to grasp larger objects and bring them up to the mouth
Some infants may show developmental signs of readiness before age 6 months, but introducing complementary foods before age 4 months – or waiting until after 6 months – is not recommended (1). Chapter 2 of the USDA Dietary Guidelines for Americans 2020-2025 encourage the introduction of potentially allergenic foods along with other complementary foods. In addition to peanuts, the Dietary Guidelines for Americans 2025 recommend eggs, cow milk products, tree nuts, wheat, crustacean shellfish, and soy be introduced when other complementary foods are introduced. Although only peanut has guideline-based recommendations for quantity and frequency (2 grams of peanut protein, 3x a week), there are currently no guideline recommendations for quantity or frequency of other allergenic foods. Looking at available studies, including the LEAP study (1), EAT study (2), and others, 2 grams of allergen protein twice a week may be a reasonable target. For foods like egg, dairy, wheat, and soy, more frequently may make sense, as these foods are ubiquitous in our diets. In the case of fish and shellfish, slightly less frequently (e.g., once a week) may equally be reasonable based on family and household consumption and accessibility.
One may determine the grams of protein by using the specification on the nutrition label of the grams of protein in a particular serving size of the food, and utilizing this measurement to calculate the goal dose of 2 grams. For the case of nut butters and sesame tahini, a little more than 2 teaspoons may be the target. In the case of egg, about 1/3 of a large egg may be the target. For fish and shellfish, in general, the serving size is about the size of the palm of a child’s hand; however, 2 grams is also the goal.
There are many factors to take into account when deciding what foods parents should introduce to their children, and when each food should be introduced. Because there are no official guidelines for most foods, it is important to utilize a shared decision-making process with the family and take into account preferences they may have. This allows for the personalized application of recommendations based on the most current and promising research. See Shared Decision Making for the Allergist for the full study (3).
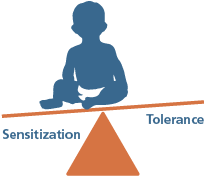
Gut vs. Skin: The Dual-Exposure Hypothesis
An important aspect to consider when deciding what foods to introduce is to consider what foods the family eats regularly, as environmental exposures to allergenic foods may be a risk factor in developing allergies. It is also important to consider what foods fit with a family’s preference, taste, and culture.
Under the dual-exposure hypothesis, if a child avoids oral exposure of an allergenic food (e.g. peanuts), but experiences frequent environmental exposures through their skin, they may be more likely to develop a sensitivity or allergy to peanut. When a child is exposed to a food allergen via the skin (e.g. food touches the skin), the immune cells of the skin are more likely to cause sensitization to that food. This is especially true if the skin is inflamed or irritated, as is the case with eczema. However, when a child is exposed to a specific food via the oral route (e.g. food is consumed), the immune cells in the digestive system create a tolerance to that food. (4,5)
Dual Exposure Hypothesis
Under the dual-exposure hypothesis, if a child does not already have an allergy and is routinely exposed to the allergen (e.g. peanut) orally, through the gut this may lead to induction of tolerance to that allergen. T-regulatory cells within mesenteric lymph nodes may play a role (lack).
Nutrition Guidance for Families
References:
- Du Toit, G., Roberts, G., Sayre, P.H., Bahnson, H.T., Radulovic, S., Santos, A.F. et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med. 2015; 372: 803–813.
- Perkin, M.R., Logan, K., Tseng, A., Raji, B., Ayis, S., Peacock, J. et al. Randomized trial of introduction of allergenic foods in breast-fed infants. N Engl J Med. 2016; 374: 1733–1743
- Blaiss MS, Steven GC, Bender B, Bukstein DA, Meltzer EO, Winders T. Shared decision making for the allergist. Annals of Allergy, Asthma & Immunology. 2019 May 1;122(5):463-70.
- Du Toit G, Sampson HA, Plaut M, Burks AW, Akdis CA, Lack G. Food allergy: Update on prevention and tolerance. Journal of Allergy and Clinical Immunology. 2018 Jan 1;141(1):30-40.
- Lack G. Update on risk factors for food allergy. Journal of Allergy and Clinical Immunology. 2012 May 1;129(5):1187-97.
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020-2025. 9th Edition. December 2020. Available at DietaryGuidelines.gov.
- Greer, F. R., Sicherer, S. H., Burks, A. W., COMMITTEE ON NUTRITION, & SECTION ON ALLERGY AND IMMUNOLOGY (2019). The Effects of Early Nutritional Interventions on the Development of Atopic Disease in Infants and Children: The Role of Maternal Dietary Restriction, Breastfeeding, Hydrolyzed Formulas, and Timing of Introduction of Allergenic Complementary Foods. Pediatrics, 143(4), e20190281. https://doi.org/10.1542/peds.2019-0281
- National Institute for Allergy and Infectious Disease. Addendum Guidelines for the Prevention of Peanut Allergy in the United States.; 2017. doi:10.1097/01.JAA.0000512231.15808.66
Test your knowledge