Cutaneous Allergen Sensitization

While early oral introduction of allergens like peanut may help induce tolerance to food, routine skin exposure to food may increase the risk of developing IgE to the food (sensitization) and ultimately the development of a food allergy (1,2,3).
Studies have demonstrated the presence of food proteins in the environment. While the majority of studies have been done with peanuts, information learned may be helpful when approaching other foods (1). There is evidence of detectable peanut protein on high touch surfaces in kitchens, detected after peanut is consumed (5). Dust samples in carpets, mattresses, and play space have also been detected (3,4,5). Peanut proteins have also been shown on hands (6) and in saliva after consuming peanut (8). All can be sources of environmental food exposures. Cleaning surfaces and hands that come in contact with peanut may assist with decreasing environmental exposures to peanut and other allergens (5,6).
Several studies have linked the presence of environmental peanut allergen and sensitization and food allergy to peanut (1,3,4,7) Although this association has been shown in those with healthy skin, eczema may increase risk (4). Skin barrier dysfunction and inflammation may be components of eczema that increase risk of sensitization to environmental food exposure. Although the majority of studies have been on peanut similar trends likely exist for other foods as well.

Consider suggesting that caregivers wash their hands before applying creams or moisturizers and prior to diaper changes, especially after handling allergens.
Dual Exposure Hypothesis
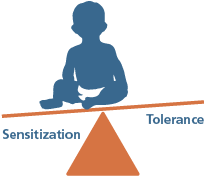
Under the dual-exposure hypothesis, if a child experiences frequent environmental exposures through their skin, but avoids oral exposure of an allergenic food (e.g. peanuts), they may be more likely to develop a sensitivity or allergy to peanut. When a child is routinely exposed to a food allergen via the skin (e.g. food touches the skin), the immune cells of the skin are more likely to cause sensitization to that food. This is especially true if the skin is inflamed or irritated, as is the case with eczema
References
- Sheehan WJ, Taylor SL, Phipatanakul W, Brough HA. Environmental food exposure: what is the risk of clinical reactivity from cross-contact and what is the risk of sensitization. The Journal of Allergy and Clinical Immunology: In Practice. 2018 Nov 1;6(6):1825-32.
- Lack G. Update on risk factors for food allergy. Journal of Allergy and Clinical Immunology. 2012 May 1;129(5):1187-97.
- Brough HA, Kull I, Richards K, Hallner E, Söderhäll C, Douiri A, Penagos M, Melen E, Bergström A, Turcanu V, Wickman M. Environmental peanut exposure increases the risk of peanut sensitization in high‐risk children. Clinical & Experimental Allergy. 2018 May;48(5):586-93.
- Brough HA, Liu AH, Sicherer S, Makinson K, Douiri A, Brown SJ, Stephens AC, McLean WI, Turcanu V, Wood RA, Jones SM. Atopic dermatitis increases the effect of exposure to peanut antigen in dust on peanut sensitization and likely peanut allergy. Journal of Allergy and Clinical Immunology. 2015 Jan 1;135(1):164-70
- Brough HA, Makinson K, Penagos M, Maleki SJ, Cheng H, Douiri A, Stephens AC, Turcanu V, Lack G. Distribution of peanut protein in the home environment. Journal of allergy and clinical immunology. 2013 Sep 1;132(3):623-9.
- Perry TT, Conover-Walker MK, Pomés A, Chapman MD, Wood RA. Distribution of peanut allergen in the environment. Journal of Allergy and Clinical Immunology. 2004 May 1;113(5):973-6.
- Brough HA, Liu AH, Sicherer S, Makinson K, Douiri A, Brown SJ, Stephens AC, McLean WI, Turcanu V, Wood RA, Jones SM. Atopic dermatitis increases the effect of exposure to peanut antigen in dust on peanut sensitization and likely peanut allergy. Journal of Allergy and Clinical Immunology. 2015 Jan 1;135(1):164-70.
- Maloney JM, Chapman MD, Sicherer SH. Peanut allergen exposure through saliva: assessment and interventions to reduce exposure. Journal of Allergy and Clinical Immunology. 2006 Sep 1;118(3):719-24.
- Northwestern Medicine. (n.d.). Infant Atopic Dermatitis Severity Scorecard: vIGA-ADTM with examples. iREACH Training Materials (Early Peanut Product Introduction Tools for Pediatric Clinicians. https://www.feinberg.northwestern.edu/sites/cfaar/docs/Pediatric%20Clinician%20Atopic%20Dermatitis%20Severity%20Scorecard2.pdf