Special Supplemental Nutrition Program for Women, Infants, and Children (WIC)
WIC serves about half of all infants born in the United States
What is WIC?
WIC, or the Special Supplemental Nutrition Program for Women, Infants and Children is a federal assistance program that serves low-income pregnant, postpartum, and breastfeeding women, infants, and children up to age 5. WIC provides these women, infants, and children with access to nutritious foods, information on healthy eating habits that include breastfeeding promotion and support, and referrals to health care.
WIC for Clinicians
What is WIC?
WIC, or the Special Supplemental Nutrition Program for Women, Infants and Children is a federal assistance program that serves low-income pregnant, postpartum, and breastfeeding women, infants, and children up to age 5. WIC provides these women, infants, and children with access to nutritious foods, information on healthy eating habits that include breastfeeding promotion and support, and referrals to health care.

Who qualifies for WIC?
In order to qualify for WIC, potential applicants must meet categorical, residential, income and nutrition risk requirements.
- Categorical Requirement:
- Pregnant women
- Breastfeeding women
- Non-breastfeeding postpartum women
- Infants
- Toddlers and children up to age 5
- Residential Requirement:
- Applicants must live in the state in which they apply.
- Applicants residing in areas where WIC is administered by an Indian Tribal Organizations (ITO) must meet residency requirements enacted by the ITO.
- Income Requirement:
- Applicants must be at or below an income level standardized by the state agency OR
- Applicants may be determined automatically income eligible based on participation in certain financial assistance programs such as:
- SNAP
- Medicaid
- Temporary Assistance for Needy Families (TANF)
- Nutrition Risk Requirement:
- “Nutrition risk” means that an individual has medical based or dietary based conditions (i.e., anemia, underweight, poor pregnancy outcome).
- Applicants must be seen by a healthcare clinician to determine whether the individual is at nutrition risk. This can be done by the applicant’s physician or in the WIC clinic at no cost to the applicant.
Applicants can also utilize the WIC Prescreening Tool to help determine if they are likely to be eligible for WIC benefits. If they are likely to be eligible, the web-based prescreening tool will provide applicants with state-specific information as well as a printable summary of their responses.
WIC: Spreading awareness
The American Academy of Pediatricians (AAP) suggests that pediatricians provide information about the nutritional and educational benefits of WIC to potentially eligible patients and families while also working collaboratively with local WIC agencies to ensure the most effective treatments and dietary guidance for patients. The AAP also recommends that pediatricians work with state and local WIC agencies to maximize efforts to promote, support, and manage breastfeeding methods for infants. Following breastfeeding guidelines goes hand in hand with the early introduction of common allergens, such as peanut. Pediatricians can help increase awareness about the benefits and resources provided by WIC by sharing information about WIC to eligible patients and families.
For more information on WIC, please visit the WIC website.
References
WIC Eligibility Requirements. USDA. (2020, June 19).
American Academy of Pediatrics. (2001, November 1). WIC Program. American Academy of Pediatrics.
U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020-2025. 9th Edition. December 2020. Available at DietaryGuidelines.gov.
For WIC Staff: Food Allergen Introduction in Infants
When should complementary foods be introduced?
USDA/HHS Dietary Guidelines for Americans recommends: At about 6 months, introduce infants to nutrient-dense complementary foods. Foods like peanuts, egg, dairy products, tree nuts, wheat, shellfish, fish, and soy should be introduced when other complementary foods are introduced.
When is my baby ready for solids?
Signs your baby is ready for solid foods:
- They can sit up.
- They can control their head and neck.
- They bring objects to their mouth.
- They swallow food instead of pushing it out.
How do I introduce possibly allergenic foods?
Start with a small tip of a spoon amount. Wait for about 10 to 15 minutes and then slowly feed the rest. Set two hours aside to watch your child. Avoid whole nuts and loose seeds as these are choking hazards. Make sure to thin out nut butters and tahini with fruit or vegetable purees, infant cereals, breast milk or formula to avoid choking.
How much allergen should I introduce?

NIAID Peanut Introduction Guidelines recommend two teaspoons of smoothed-out peanut butter (about 2 grams of peanut protein) three times a week. At this time there are no quantitative guidelines for other allergenic foods, but consider a goal of 2 grams of the food protein twice a week (e.g. 1/3 of an egg or 2 tsp of smoothed-out nut butters/tahini).
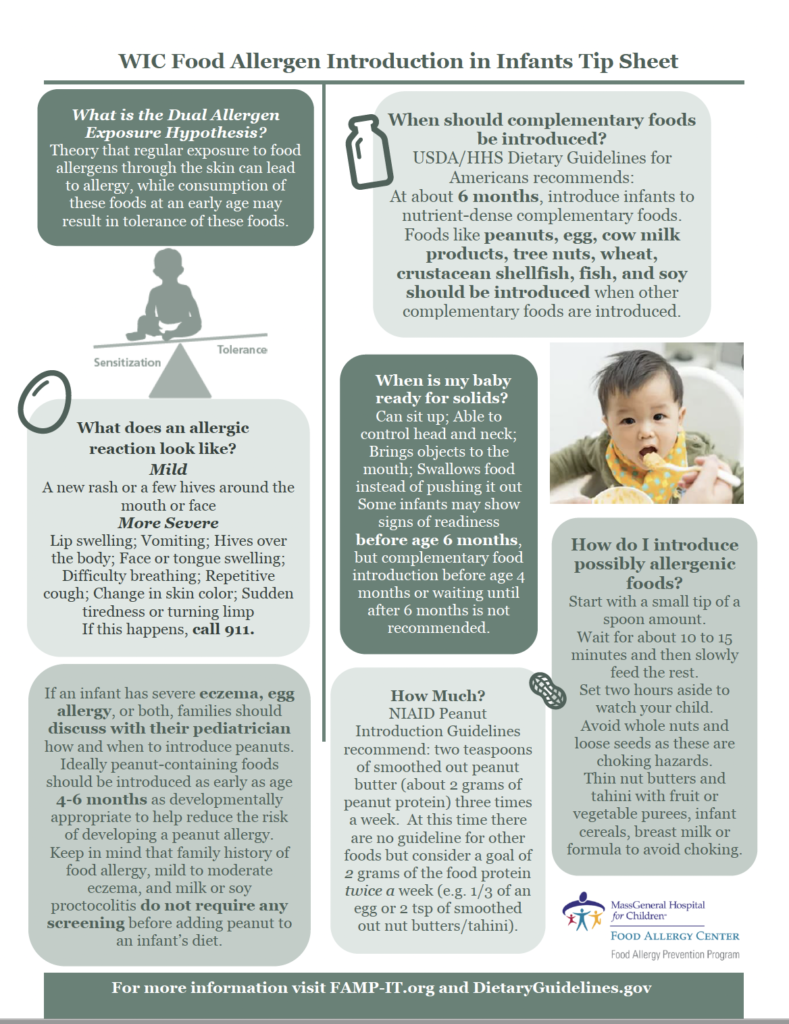
What is the Dual Allergen Exposure Hypothesis?
The theory that regular exposure to food allergens through the skin can lead to allergy, while consumption of these foods at an early age may result in tolerance of these foods.
What does an allergic reaction look like?
Mild reaction:
- A new rash or a few hives around the mouth or face.
More severe reaction:
- Lip swelling
- Vomiting
- Hives over the body
- Face or tongue swelling
- Difficulty breathing
- Repetitive cough
- Change in skin color
- Sudden tiredness or turning limp
If this happens, call 911.
If an infant has severe eczema, egg allergy, or both, families should discuss with their pediatrician how and when to introduce peanuts. Ideally, peanut-containing foods should be introduced as early as age 4-6 months as developmentally appropriate to help reduce the risk of developing a peanut allergy. Keep in mind that family history of food allergy, mild to moderate eczema, and milk or soy proctocolitis do not require any screening before adding peanut to an infant’s diet.
Massachusetts WIC Program Advanced Nutrition Training: Food Allergy Prevention (Archived Training; October 20, 2022)
Video 1: Training Webinar
Video 2: Cases and Q+A
Test your knowledge
© 2024 MassGeneral Hospital for Children Food Allergy Center. All rights reserved.